Is Your Headache a Migraine?

A migraine is a headache with throbbing pain that is usually worse on one side of the head. The pain is often severe enough to hamper daily activities and may last from four hours to three days if untreated. More than one in 10 Americans, including one in 6 women, have migraines, but many have been told mistakenly that they have a sinus or tension headache. Foods, stress, and hormones can be migraine triggers.
Throbbing pain typically occurs on one side near the temples, forehead, and eyes. Migraine headaches can make you very sensitive to light, sound, or mild exertion, such as climbing the stairs. Many people have nausea, vomiting, or vision problems. The pain can be disabling, forcing people to miss work or other activities.

About 20% of people who suffer from migraine headaches will have an aura about 20 minutes to an hour before the pain. They may see flashing lights, wavy lines, or dots, or they may have blurry vision or blind spots. These are called "classic migraine headaches."
Some people may have a change in mood before a migraine begins. They may become more excitable or irritable or depressed. Others may detect a sensation, such as a funny smell or taste. They may feel more fatigued, yawn frequently, or experience muscle tension. About 1 in 4 people experience this prodrome phase, which can occur as early as 24 hours before any head pain.
The exact cause of migraine headaches is still not well understood, but the problem is considered to be neurological (related to the nervous system). It is believed that brain chemicals, blood vessels, and nerves of the brain are involved.

Migraine headaches may be set off by some specific cause, such as flickering lights. This could be a reflection from snow or water or from fluorescent bulbs or television or movie screens. Wearing polarizing sunglasses outside and using daylight spectrum fluorescent bulbs inside may help.
Emotional stress is a common trigger of migraine headaches. While it's impossible to completely avoid stress, relaxation exercises can help you cope. Inhale and exhale slowly, letting the air fill you and then deflate like a balloon. Some people find that thinking of a peaceful scene or listening to favorite music can help.

It's important for people prone to migraine headaches to have a regular pattern of meals and sleep. Low blood sugar from skipping meals can trigger a migraine. Eating too much sugar also can cause a spike, then a "crash" in blood sugar. Drink water throughout the day to avoid dehydration and sleep at least six to eight hours a night.

For many women, migraine headaches are tied to their menstrual cycle, occurring either a few days before or during their period, when estrogen levels drop. Some women may benefit from anti-inflammatory medication before their headaches begin, or hormonal birth control such as pills, patches, or rings. Others may have no benefit or worse migraine headaches with hormonal birth control.

Migraine sufferers often report that certain foods trigger their headaches. Common culprits include MSG, red wine, cheese, chocolate, soy sauce, and processed meats. However, scientific studies haven't confirmed any particular food as a migraine trigger.

Aged, fermented, and stored foods have higher levels of tyramine, a substance created from the breakdown of the amino acid tyrosine. Tyramine may cause blood vessels to constrict then expand, and it may be a trigger for some migraine headaches. Some headache experts advise limiting fermented or aged foods, such as cheese, soy sauce, pickles, and pepperoni.

When combined with some pain medications, caffeine can help provide relief. Most migraine sufferers can drink a cup or two a day of coffee without any problems. However, too much caffeine can lead to headaches when the stimulant effect wears off.
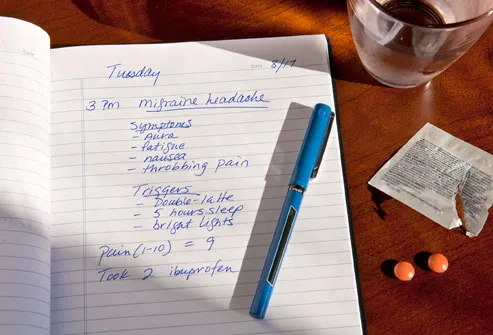
Find out what triggers migraine headaches by keeping a headache diary. Each time you suffer from a migraine, make a note about the warning signs (the "prodrome"), triggers, and severity. If you can discover some of your personal triggers, you may be able to avoid future headaches.

Women are three times more likely to have migraine headaches than men. If you have a close relative with migraine, you are much more likely to have them, too. Experts believe migraine may be related to mutations in genes that affect certain areas of the brain. Migraine headaches are also more common among people who have epilepsy, depression, asthma, anxiety, stroke, and some other neurologic and hereditary disorders.

About 5% of the children with headache problems suffer from migraine headaches. Both boys and girls can get migraine headaches, but after puberty they are more common among girls. Children may have symptoms other than headache, including stomach pain (abdominal migraine) or forceful and frequent vomiting (cyclic vomiting). If young children become wobbly on their feet, pale, and fussy, or have involuntary eye movements or vomiting, they may have a form of migraine called benign paroxysmal vertigo.

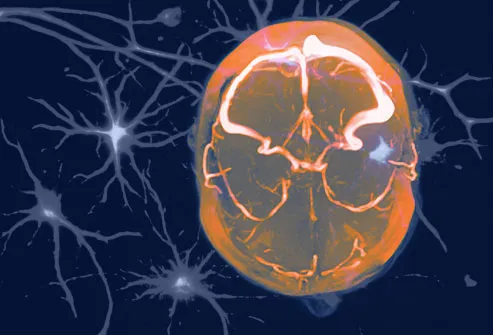
Migraine headaches are diagnosed primarily from symptoms, but your doctor may want to do a brain scan to rule out other causes of headaches, such as a brain tumor or bleeding in the brain. A CT scan uses special X-rays to create cross-sectional images of the brain. An MRI uses radio frequency pulses and a magnetic field to create images of the brain.

Before you begin treatment, your doctor may want to assess your "headache burden" -- how much your life is affected by migraine headaches. A simple questionnaire asks how many times you have missed work, school, or family or leisure activities because of headaches.

Combinations of common pain relievers and anti-inflammatories may help: acetaminophen, aspirin, ibuprofen, naproxen sodium. Some have been formulated specifically to treat migraine headaches. However, overuse may actually make headaches worse or may lead to ulcers or other gastrointestinal problems.

Triptans, the most common medication prescribed for migraine headaches, are most effective when taken early in an attack. Common triptans include Amerge, Axert, Frova, Imitrex, Maxalt, Relpax, Treximet, and Zomig. People with high blood pressure, heart disease, stroke, and other conditions may not be able to take triptans. And because of possible serious drug interactions, you should talk to your doctor about other medications you take, such as antidepressants or antiseizure drugs. Side effects of triptans include nausea, dizziness, tingling, numbness, and chest pain.

If triptans don't give you relief, your doctor may prescribe dihydroergotamine (Migranal) or ergotamines (Cafergot or Migergot) as tablets, nasal sprays, or injections. These drugs narrow the blood vessels and can cause nausea, dizziness, muscle pain, or a bad taste in the mouth. They are not usually as effective as triptans and also have some interactions with other drugs.

After you have treated two or three headaches, ask yourself some simple questions. Are you getting the relief you need? If not, you should ask your doctor about altering treatment. Be sure you take medications early in the attack -- at least within two hours of migraine pain.

Overuse of medications can sometimes lead to chronic headaches. You shouldn't take prescribed medication more than two times per week. You can get rid of the chronic headaches by tapering and discontinuing medication -- under a doctor's supervision. Pain medicines containing narcotics should be taken at the direction of physician because they can be habit-forming.

If migraine headaches are frequent or very severe, you may need to take a drug every day to prevent attacks. Drugs used to treat high blood pressure can be prescribed for this purpose. They include beta blockers and calcium channel blockers. Several types of antidepressants can also be used to prevent migraine, as well as anticonvulsants. Even Botox, which is normally used to treat wrinkles, can keep migraines at bay for some people.
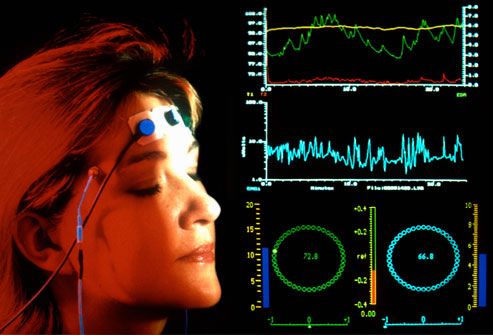
Biofeedback and relaxation training can give you relief that is similar to the help you get from medications. Biofeedback uses a monitor to train you to recognize the onset of muscle tension and changes in body temperature that are signals of stress.

Acupuncture is a form of Chinese medicine that uses very fine needles inserted in specific spots to balance the body's energy flow. Some researchers have found acupuncture causes the brain to release chemicals that affect pain. However, studies on the effectiveness of acupuncture for migraine symptoms has been mixed.

Migraine headaches most often strike in the prime of life – between the ages of 20 and 60. While elderly people still get migraine headaches, they often decrease in severity and frequency as we age, or even disappear entirely. Good management of migraines may help you get rid of migraine headaches for good.

Any new headache that is unusually severe or lasts more than a couple of days should be checked by a doctor. It's also important to let your health care provider know if the pattern of headaches changes -- for example, if there are new triggers. If you have a headache accompanied by paralysis, confusion, fever, or stiff neck, seek emergency medical care.