Anatomy of Depression
It's natural to feel down sometimes, but if that low mood lingers day after day, it could signal depression. Major depression is an episode of sadness or apathy along with other symptoms that lasts at least two consecutive weeks and is severe enough to interrupt daily activities. Depression is not a sign of weakness or a negative personality. It is a major public health problem and a treatable medical condition.
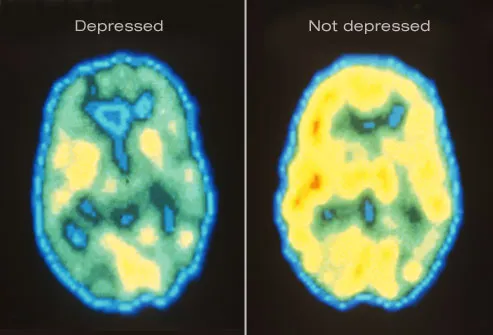
Shown here are PET scans of the brain showing different activity levels in a person with depression, compared to a person without depression.

The primary symptoms of depression are a sad mood and/or loss of interest in life. Activities that were once pleasurable lose their appeal. Patients may also be haunted by a sense of guilt or worthlessness, lack of hope, and recurring thoughts of death or suicide.

Depression is sometimes linked to physical symptoms. These include:
o Fatigue and decreased energy
o Insomnia, especially early-morning waking
o Excessive sleep
o Persistent aches or pains, headaches, cramps, or digestive problems that do not ease even with treatment
Depression can make other health problems feel worse, particularly chronic pain. Key brain chemicals influence both mood and pain. Treating depression has been shown to improve co-existing illnesses.

Changes in appetite or weight are another hallmark of depression. Some patients develop increased appetite, while others lose their appetite altogether. Depressed people may experience serious weight loss or weight gain.

Without treatment, the physical and emotional turmoil brought on by depression can derail careers, hobbies, and relationships. People with depression often find it difficult to concentrate and make decisions. They turn away from previously enjoyable activities, including sex. In severe cases, depression can become life-threatening.

People who are depressed are more likely to attempt suicide. Warning signs include talking about death or suicide, threatening to hurt people, or engaging in aggressive or risky behavior. Anyone who appears suicidal should be taken very seriously. Do not hesitate to call one of the suicide hotlines: 800-SUICIDE (800-784-2433) and 800-273-TALK (800-273-8255). If you have a plan to commit suicide, go to the emergency room for immediate treatment.

Anyone can become depressed, but many experts believe genetics play a role. Having a parent or sibling with depression increases your risk of developing the disorder. Women are twice as likely as men to become depressed.
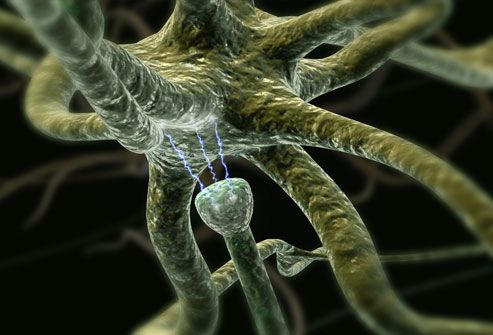
Doctors aren't sure what causes depression, but a prominent theory is altered brain structure and chemical function. Brain circuits that regulate mood may work less efficiently during depression. Drugs that treat depression are believed to improve communication between nerve cells, making them run more normally. Experts also think that while stress -- such as losing a loved one -- can trigger depression, one must first be biologically prone to develop the disorder. Other triggers could include certain medications, alcohol or substance abuse, hormonal changes, or even the season.
Illustrated here are neurons (nerve cells) in the brain communicating via neurotransmitters.

If your mood matches the season -- sunny in the summer, gloomy in the winter -- you may have a form of depression called seasonal affective disorder (SAD). The onset of SAD usually occurs in the late fall and early winter, as the daylight hours grow shorter. Experts say SAD affects from 3% to 20% of all people, depending upon where they live.

The "baby blues" strikes as many as three out of four new mothers. But nearly 12% develop a more intense dark mood that lingers even as their baby thrives. This is known as postpartum depression, and the symptoms are the same as those of major depression. An important difference is that the baby's well-being is also at stake. A depressed mother may have trouble enjoying and bonding with her infant.

In the United States, depression affects 2% of grade school kids and about one in 10 teenagers. It interferes with the ability to play, make friends, and complete schoolwork. Symptoms are similar to depression in adults, but some children may appear angry or engage in risky behavior, called "acting out." Depression can be difficult to diagnose in children.

As of yet, there is no lab test for depression. To make an accurate diagnosis, doctors rely on a patient's description of the symptoms. You'll be asked about your medical history and medication use since these may contribute to symptoms of depression. Discussing moods, behaviors, and daily activities can help reveal the severity and type of depression. This is a critical step in determining the most effective treatment.

Studies suggest different types of talk therapy can fight mild to moderate depression. Cognitive behavioral therapy aims to change thoughts and behaviors that contribute to depression. Interpersonal therapy identifies how your relationships impact your mood. Psychodynamic psychotherapy helps people understand how their behavior and mood are affected by unresolved issues and unconscious feelings. Some patients find a few months of therapy are all they need, while others continue long term.

Antidepressants affect the levels of brain chemicals, such as serotonin and norepinephrine. There are many options. Give antidepressants a few weeks of use to take effect. Good follow-up with your doctor is important to evaluate their effectiveness and make dosage adjustments. If the first medication tried doesn't help, there's a good chance another will. The combination of talk therapy and medication appears particularly effective.

Research suggests exercise is a potent weapon against mild to moderate depression. Physical activity releases endorphins that can help boost mood. Regular exercise is also linked to higher self-esteem, better sleep, less stress, and more energy. Any type of moderate activity, from swimming to housework, can help. Choose something you enjoy and aim for 20 to 30 minutes four or five times a week.
Light therapy has shown promise as an effective treatment not only for SAD but for some other types of depression as well. It involves sitting in front of a specially designed light box that provides either a bright or dim light for a prescribed amount of time each day. Light therapy may be used in conjunction with other treatments. Talk to your doctor about getting a light box and the recommended length of time for its use.

St. John's wort is an herbal supplement that has been the subject of extensive debate. There is some evidence that it can fight mild depression, but two large studies have shown it is ineffective against moderately severe major depression. St. John's wort can interact with other medications you may be taking for medical conditions or birth control. Talk to your doctor before taking this or any other supplement.

A playful puppy or wise-mouthed parrot is no substitute for medication or talk therapy. But researchers say pets can ease the symptoms of mild to moderate depression in many people. Pets provide unconditional love, relieve loneliness, and give patients a sense of purpose. Studies have found pet owners have less trouble sleeping and better overall health.

Because loneliness goes hand-in-hand with depression, developing a social support network can be an important part of treatment. This may include joining a support group, finding an online support community, or making a genuine effort to see friends and family more often. Even joining a book club or taking classes at your gym can help you connect with people on a regular basis.

Vagus nerve stimulation (VNS) can help patients with treatment-resistant depression that does not improve with medication. VNS is like a pacemaker for the brain. The surgically implanted device sends electrical pulses to the brain through the vagus nerve in the neck. These pulses are believed to ease depression by affecting mood areas of the brain.

Another option for patients with treatment-resistant or severe melancholic depression is electroconvulsive therapy (ECT). This treatment uses electric charges to create a controlled seizure. Patients are not conscious for the procedure. ECT helps 80% to 90% of patients who receive it, giving new hope to those who don't improve with medication.

A newer option for people with stubborn depression is repetitive transcranial magnetic stimulation (rTMS). This treatment aims electromagnetic pulses at the skull. It stimulates a tiny electrical current in a part of the brain linked to depression. rTMS does not cause a seizure and appears to have few side effects. But doctors are still fine-tuning this treatment.

In the midst of major depression, you may feel hopeless and helpless. But the fact is, this condition is highly treatable. More than 80% of people get better with medication, talk therapy, or a combination of the two. Even when these therapies fail to help, there are cutting-edge treatments that pick up the slack.