Drug Addiction, Social Connection, and the Brain
A new study of opioids reveals a tie between drug addiction and social connection.
Science has long known that having positive social connection is important to a happy and healthy life. But less is understood about how our brains support and encourage connecting with others.
While prior research has suggested oxytocin plays a role in nurturing and trusting others, thereby strengthening social bonds, many researchers also suspect that brain opioids are important to social connection. Opioids are naturally occurring brain chemicals—perhaps the most well-known being endorphins—that cause pleasurable sensations in the body and encourage us to enjoy whatever we are experiencing. It’s possible that opioids also cause the warm feelings we get in social encounters, thereby encouraging us to be more engaged with others.
But, according to a recent study, the role of opioids may be a little more complicated than that—and there are practical implications for how we treat drug addiction.
Opioids target social connection
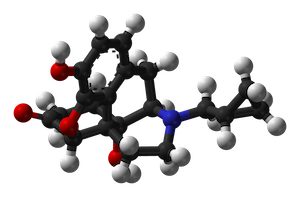 Naltrexone, a medication that inhibits opioids
Naltrexone, a medication that inhibits opioids
Participants unaware of the study’s purpose took an opioid inhibitor called naltrexone for a four-day trial and a placebo for another four-day trial in randomized order, with a break in between to clean out their system.
Over the course of the experiment, the participants kept daily track of how socially connected they felt and how positive their moods were. On the fourth day of each trial, they completed a task in the lab, reading six very kind messages that loved ones had sent to the researchers in advance, unbeknownst to the participants—messages like “I am so grateful to have you in my life” and “Thank you for loving me at my worst.” Then participants reported how connected they felt toward the message writer, as well as how good it felt to read the messages.
Afterwards, the researchers compared how much social connection participants had in their everyday lives, as well as how much of a sense of connection they felt during the lab task. Results showed that participants felt more connection in both everyday activities and during the lab task when they were on placebo than when on naltrexone, suggesting that naltrexone was blocking opioids important to social closeness.
“We tested a long-standing theory—based on animal data—that suggests brain opioids contribute to feelings of connection. But no one had shown that relationship causally in humans,” says the study’s lead author, Tristen Inagaki.
She and her colleagues also found that taking naltrexone did not decrease positive emotion in everyday life, even though it affected the participants’ sense of connection to others. This suggests that opioids play a targeted role in social connection that is above and beyond just feeling good.
“All of this work is trying to get at what makes us feel connected to others and how we can help those who are feeling lonely or socially isolated.”
“Opioids seem to affect our response to the most rewarding or most pleasurable stimuli in the environment,” says Inagaki. “For humans, being social or being around your loved ones is likely to be the most salient rewarding stimuli.”
Inagaki points to other research showing that opioids reduce the sense of connection people get from simply holding a warm object, but don’t affect ratings of pleasure. This lends further support to her own findings.
“The mechanisms for opioids must be smarter than we think,” she says.
The addiction connection
While much of the research on opioids and social connection is preliminary, Inagaki thinks her study warrants attention, given that opioid inhibitors like naltrexone are often used with patients to treat addictions. Though naltrexone may indeed inhibit the high people feel when taking illicit drugs—and thereby help them kick the habit—it may also shape their social relationships.
“Lots of research shows that people really need their social networks when they’re dealing with major stressors—addiction being a major stressor,” says Inagaki. “So, if the drug prescribed to help someone overcome addiction is also reducing how connected they feel toward others or reducing the time they spend with other folks, that’s not a great outcome.”
At the very least, she says, clinicians should be aware of the potential downside of using naltrexone, so they can warn patients about social side effects and make sure patients are remaining socially integrated.
While Inagaki’s findings are intriguing in their own right, they may also be relevant to understanding the current opioid addiction. Research has shown that genetic differences in opioid receptors lead to increased risk of addiction, just as her research suggests blocking opioid receptors decreases social closeness. Doesn’t that suggest feelings of disconnection and addiction could be related?
Inagaki thinks so.
Inagaki thinks so.
“One offshoot of the opioid theory is that those with low opioid tone show exaggerated responses to social stressors—like feeling lonely, feeling socially rejected,” she says. “So, the idea that negative social encounters could produce a risk factor for all kinds of mental health issues, including addiction, is being re-appreciated right now.”
While the jury is still out, Inagaki and her team will continue to research the role that opioids play. She is currently running a neuroimaging study to see how naltrexone impacts neural activity in response to social connection. She hopes that her research will help inform how we humans bond, with implications beyond addiction.
“All of this work is trying to get at what makes us feel connected to others and how we can help those who are feeling lonely or socially isolated,” she says. “My hope is that people who are struggling don’t have to turn to drugs.”