How to Turn Stigma about Mental Illness into Compassion
Stephen Hinshaw explores what it meant to be raised by a father with psychosis—and how that experience has informed his work as a psychologist.
What is it like to grow up in a household with a parent displaying serious mental illness?
Renowned psychologist Stephen Hinshaw knows firsthand. His father suffered major bouts of psychosis that kept him periodically hospitalized during Hinshaw’s childhood. Yet, the reasons for these absences were never explained to Hinshaw, until he turned 18 and his philosopher father started to divulge his lifetime of struggles (which included being (mis)diagnosed with schizophrenia for decades).
 Stephen Hinshaw
Stephen Hinshaw
Hinshaw is now a professor of psychology at the University of California, Berkeley, and an internationally recognized expert on developmental psychopathology. He has written a memoir about his experiences of growing up in a family where mental illness was hidden.
His book, Another Kind of Madness: A Journey through the Stigma and Hope of Mental Illness, is brutally honest, divulging his father’s plight as well as his own struggles with mental illness—including depression, obsessive thinking, and troubled eating patterns. Even more, it’s a call to action to stop the silence surrounding mental illness and to prevent stigmatization, so that people can get the treatment and support they need.
I sat down with him to ask more about his experiences and what they might teach the rest of us.
Jill Suttie: Why did you decide to write this memoir?
Stephen Hinshaw: I thought my dad’s story—and that of my whole family—was an important one. To overcome the shame and stigma associated with mental illness, we need to tell honest stories about families who were silenced, and bring to light what so many families go through. Mental illness isn’t rare—it occurs frequently—and when it gets treated, things can really change for the better. But treatment won’t be sought if there’s shame about the entire issue. Encouraging open discussion is the key reason for this book.
JS: How did the silence you experienced around your father’s illness affect you as a child?
SH: It’s hard to recall precisely, because of the “haze” surrounding my Dad’s absences; but I remember thinking, If only I were a better kid, maybe Dad wouldn’t go away next time.
So, I blamed myself. Kids do this when there are family problems but nothing is said. Now, with the hindsight of my career as a developmental psychologist, I understand that this kind of silence breeds internalization. In other words, it may be better to blame yourself—though often at a big cost to self-esteem, plus adding vulnerability to depression later on—than believing the world is just cruel and random. At least you maintain some sense of control.
Major depression has a substantial genetic liability that’s even stronger for bipolar disorder. Yet, as my colleague Bill Beardslee of Harvard Medical School has found out through randomized clinical trials, in families where parents have depression or bipolar disorder, if a family therapist gets the family to talk with their kids about these experiences, things can improve, often dramatically. Not only do kids participating in this kind of treatment function better at the end of the treatment, but even four years later, their own risk of depression is cut in half.
Talking and communicating as a family may prevent the internalization that’s too often a part of the intergenerational transmission of mental illness.
JS: When your father finally talked to you to explain his illness, what was that like?
SH: It was like I’d been holding my breath for 18 years and I was low on oxygen. Then, all of a sudden, an air vent opened.
My dad and I talked about his experiences three or four times a year after our first discussion. Initially, though, I didn’t tell roommates, girlfriends, classmates, or anybody about what I was learning, because I was afraid that I would end up as flawed as my dad.
Stigma goes deep; shame goes deep. Gradually, when I dared speak up, trusted friends said “Tell me more.” It’s like anything in life where you need some support: once you make the effort to reach out and people don’t shun you, your world opens up.
Life really changed for me, once I was able to come out of the closet. The antidotes to what is often called self-stigma, or internalized stigma, are finding a group you can relate to, having a voice, and taking social action. Self-stigma isn’t inevitable if there’s solidarity, if there’s kinship.
JS: What is the role of stigma in seeking treatment for mental illness or even in the treatment itself?
SH: Mental illnesses can be extremely costly in terms of symptoms and impairments, especially for conditions like major depression, bipolar disorder, schizophrenia, Obsessive Compulsive Disorder, and PTSD, as well as a host of child-onset disorders (ADHD, autism, etc.). Unless evidence-based treatment is sought and received, problems can linger and fester.
There’s a crucial reason why so many people don’t seek treatment…or that evidence-based treatments aren’t sufficiently available…or that therapists aren’t well trained in them. It’s stigma—the shame surrounding the entire topic. Some people say we shouldn’t talk about the stigma of mental illness, because there’s nothing to be ashamed about. Well, that’s kind of like saying we shouldn’t use the word racism. It still exists even though we’ve made progress.
But too often, mental illnesses are considered to be diseases you bring on yourself, because of poor character or weak will. Or, as has been believed in traditional cultures, because of animal spirits or evil spirits. Today, we know that mental illness can be treated—it’s a disease with origins in the brain—and that’s real progress. Yet if the public is led to believe that mental illness is produced exclusively by one’s genes, pessimism rules—after all, their very DNA is flawed—and social distance increases.
Like most modern illnesses, genetic risk and biological factors are clearly involved in mental disorders. But lifestyle and health choices, along with the decision to engage in treatment, are also crucial. We still don’t have parity for mental health treatment compared to physical health treatment—too often, it’s still a taboo topic.
JS: How do you get around such stigma, to be able to help people?
SH: That’s the 64-jillion-dollar question. These are complex illnesses in the way that cancer, diabetes, and coronary artery disease are complex. Genetic vulnerability exists, yet certain early life experiences can make a person more at risk.

I’m really interested in helping young people to overcome stigma. If you go into health classes in middle schools or high schools and teach the “facts” about mental illness, we know from research that kids will learn such factual information—but, at the same time, their stigma is likely to increase.
Why? Facts, out of context, tend to reinforce the wrong stereotype. The knowledge that needs to be transmitted is that, with proper treatment, people with bipolar disorder or PTSD can really improve.
One of the great social psychologists, Gordon Allport, who wrote The Nature of Prejudice, said that you can teach and you can preach; but if you’re not in contact with the outgroup—the other tribe, the people we think of as lesser somehow—then you won’t understand that they’re human just like you.
This is what we’re doing in a growing number of high schools in the Bay Area, evaluating something called LETS—Let’s Erase The Stigma. Kids join the LETS club and meet once a week with a club advisor to discuss mental illness in themselves or family members or friends. Topics like bullying and “difference” are also on the table.
In our first batch of research, we found that this kind of youth-directed intervention, guided by contact and social action, reduces “social distance” and improves attitudes, even if it doesn’t teach all that much about mental illness facts.
JS: How did your own bouts of mental illness impact your work and research? Do you feel they made you more compassionate?
SH: It’s a sad fact that if you ask people with serious mental illness about their lives and what they find stigmatizing, one of the top responses is, I’m stigmatized by the mental health profession’s low expectations. For example, my doctor may tell me I’ll never get a real job. Or worse. In fact, how have people in the mental health and health professions usually been trained? We’re right, and the patients are wrong; we’re healthy and they’re sick—an “us versus them” mentality.
But coming to understand my Dad, and other family members, as well as my own doubts, made me more sensitive and compassionate, I’m sure. Unless it’s cripplingly severe, depression can give you compassion and empathy. I had the kinds of experiences to counteract some of the professional training I received.
Over the years, blessed by my family’s strengths and my own drive, I worked as hard as I could in college, in running summer camps and schools for troubled kids, in grad school, and throughout my teaching and research career. What a fascinating life I’ve had—with a real chance to give back!
Essential for overcoming stigma is the ability to be open—and to get support. For me, seeing a therapist has been crucial as well.
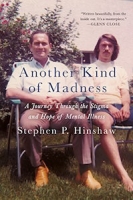 Another Kind of Madness: A Journey through the Stigma and Hope of Mental Illness(St. Martin's Press, 2017, 288 pages)
Another Kind of Madness: A Journey through the Stigma and Hope of Mental Illness(St. Martin's Press, 2017, 288 pages)
JS: What can we do personally to help someone we know with mental illness?
SH: The core theme is that if you stick your head in the sand, ignore it, and think it’ll go away, things will almost always backfire.
SH: The core theme is that if you stick your head in the sand, ignore it, and think it’ll go away, things will almost always backfire.
Number one, don’t be afraid to talk about it. People need social support—and knowing there’s an accepting family or community of workers or friends around is crucial. Number two, you may have to learn more about mental illness. It can seem mysterious or scary; but it’s important to learn what you can about symptoms of mental illness and which treatments can really help. Number three: get them to seek professional help if symptoms are more than transitory. Therapy, and when needed, medication, are effective when good professionals are involved.
JS: What do you think we as a society need to do to prevent stigma?
SH: How do we overcome racial prejudice? How do we prepare for the ecological changes befalling our planet? How do we enact any major social change?
Well, I think it’s a mistake to think that there’s just one strategy. These are multi-level problems.
In terms of stigma, one way is to work top down. For example, the Americans with Disabilities Act (ADA) became law in 1990, making it illegal, in public spaces or the workplace, to discriminate against somebody with a physical or mental disability.
That’s great, but what often happens in the workplace? People don’t want to tell anyone about their mental illness. If they do, they fear they won’t be hired or they’ll be fired. Ninety-five-plus percent of the lawsuits brought under ADA are from people with physical disabilities—to get a ramp put in, or wider bathroom entrances. Under 5 percent of claims are filed for mental disorders.
The paradox here is that the accommodations needed for somebody with a mental illness are often minor—things like flex time to see your psychologist during lunch. The cost to the organization is miniscule, but people are too afraid of the shame and stigma to even ask for it. There needs to be support for individuals with mental illness to dare to disclose.
Contact and support are urgently needed, including empathy on the part of the general public. We need to change media images. We did a study on how mental illness is portrayed in the media—with coders blind to what we were looking for—and found little change in how mental illness has been portrayed over the last 25 years in major newspapers.
Now, that seems wrong. There are television shows—Carrie on Homeland, for example—that give more accurate portrayals of, for example, bipolar disorder, than ever before. But, by and large, the two main stereotypes in the media are violence and incompetence.
In the end, we need stories of everyday struggles, everyday triumphs. This is what has made cancer such a cause now—knowing it’s your aunt, your sister, your workmate who’s struggling with breast cancer. It engages people’s empathy when they hear stories about everyday people struggling and coping, with humor and tragedy and triumph.
We still don’t have enough of that with mental illness. So, this is the reason for Another Kind of Madness: to convey a deeply personal narrative, with the goal of humanizing the entire topic. In fact, I believe that humanization is the ultimate “cure” for stigma.